|
|
What is colonoscopy?
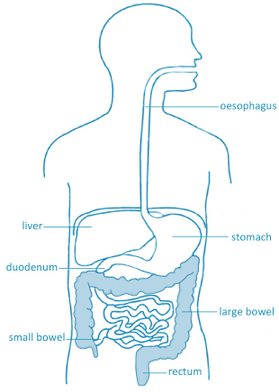
A colonoscopy is a safe and effective way of visually examining the lining of the large bowel. It is performed by a gastroenterologist to diagnose and in some cases, treat problems of the lower digestive system.
A colonoscope is a thin, flexible tube with a tiny video camera and a light on the end. By adjusting the various controls on the colonoscope, your gastroenterologist can safely guide the instrument to look at the inside of the colon. A colonoscopy is used to look closely for any problems that may require evaluation, diagnosis or treatment. This may include the taking of biopsies (tissue samples), or the removal of polyps (abnormal growths), which may otherwise become bowel cancers. What is the reason for having a colonoscopy?
A colonoscopy is a safe and effective way to evaluate problems such as blood loss, pain, changes in bowel habit, or abnormalities that may have first been detected by other tests.
Common reasons for having a colonoscopy include:
- A persisting change in bowel function - Rectal bleeding - A family history of bowel cancer - A personal history of colonic polyp - Unexplained abdominal symptoms or weight loss If it is unclear to you why your GP has recommended a colonoscopy, we encourage you to book another appointment with them to discuss this further. Does it reduce my risk of developing colon cancer?The incidence of colon cancer and related deaths is reduced by colonoscopy in patients at high risk of colon cancer. This benefit depends on an individual’s cancer risk (eg. family history) and may not directly relate to you – the benefit of colonoscopy for you should be discussed directly with your doctor.
With colonoscopy, it is now possible to detect and remove most polyps in the colon without the need for surgery. Not all polyps are pre-cancerous but it is not possible to tell just by looking at a polyp if it will become a cancer. For this reason, all polyps are usually removed when found. Is there an alternative to having a colonoscopy?
Depending on the reason your doctor has suggested a colonoscopy, there may be alternative tests available. You can discuss these options with your doctor. Alternative tests may include:
How do I prepare for the procedure?
It is very important that the bowel is cleared before your colonoscopy. This is the most challenging part of the whole process and is done the day before your procedure using laxatives. It is essential that you complete this step carefully because how well the bowel is emptied determines the success of the procedure. Please read our ‘Colonoscopy Preparation Instructions' here.
Can I take my usual medications prior to the procedure?
Do I have to fast for the procedure?
Please review the bowel preparation instructions. You need to completely fast for 6 hours prior to the procedure.
What do I need to bring on the day of my procedure?
Please bring your doctor’s referral letter if available, health fund details and Medicare card. Please wear loose fitting clothing that can be easily removed - you may need to change into a patient gown. Any jewellery and valuables should be left at home.
What happens when I arrive at hospital?You will be asked some basic questions about your health and medications. You will be asked to sign a form to verify your consent for the procedure and understanding of what is involved. You will have the opportunity to meet the anaesthetic doctor and gastroenterologist before the procedure begins to go through any questions that have arisen.
What will happen during the procedure?During the procedure, every effort will be made to ensure you are as comfortable as possible. You will be asked to change into a hospital gown. You will also be asked to remove glasses, jewellery and any contact lenses.
A cannula (small needle) will be placed into the back of your hand through which sedative medication will be given. You will be asked to lie on your side on the hospital bed before the anaesthetic doctor gives you sedation. Your blood pressure, pulse and oxygen level will be carefully monitored throughout the procedure. The sedative medication will put you into a deep sleep so that you will be comfortable. The colonoscope will then be passed through your rectum around the colon and when possible advanced into the last part of the small bowel. Air is pumped through the colonoscope to expand the colon so that it is easier to visualise. If necessary, biopsies and/or polyps with be taken/removed – this does not cause any pain. How long will the procedure take?
The time needed for colonoscopy varies but on average the procedure takes 15-30 minutes. It is usually done as a day procedure so you will not have to stay overnight in hospital.
What will happen after the colonoscopy?Your specialist will speak with you after your procedure before you go home. If any biopsies are taken or polyps removed, the results for these will take several days to be processed and an arrangement for follow-up with your GP will be needed. You will also be given instructions regarding how soon you can eat and drink, plus other guidelines for resuming your normal activity.
You cannot drive, drink alcohol, sign legal documents or operate machinery for the first 24 hours after your procedure. This is because the sedative medication you received may affect your concentration or coordination. When will I be able to go home?You will be ready to go home about 2 hours after the procedure. You will need someone to drive you home. It is best for someone to stay with you for the first 24 hours.
Most patients do not have any problems after the procedure but if you develop severe abdominal pain, fevers or chills, have difficulty breathing, persistent bleeding (more than half a cup) or any other symptoms that you are concerned about in the hours or days after the colonoscopy, you should contact your doctor (or the closest emergency department). What are the risks of having a colonoscopy?Colonoscopy is a common procedure that is generally safe and very well tolerated.
Common temporary side-effects include:
Complications are very rare, but may include:
If you wish to discuss the details of all possible rare complications, you should inform your doctor and/or anaesthetist prior to the procedure. Exact risks will differ for every person – so ask your doctor how these risks apply to you. |